
Endometriosis - A must-know guide to a common, yet little known and misunderstood condition
Endometriosis is a chronic condition that affects millions of women worldwide, yet remains poorly understood and often misdiagnosed.
Despite its prevalence, many misconceptions continue to circulate, creating confusion for those seeking help.
This guide aims to dispel myths about endometriosis while providing clear, evidence-based information about its symptoms, causes, and treatment options.
What is endometriosis?
Endometriosis occurs when tissue similar to the lining of the uterus (the endometrium) grows outside the uterus. In endometriosis, this tissue can be found on the ovaries, fallopian tubes, and other organs in the pelvic region, and sometimes even beyond.
Just like the tissue inside the uterus, these growths respond to hormonal changes during the menstrual cycle, leading to inflammation, scarring, and pain.
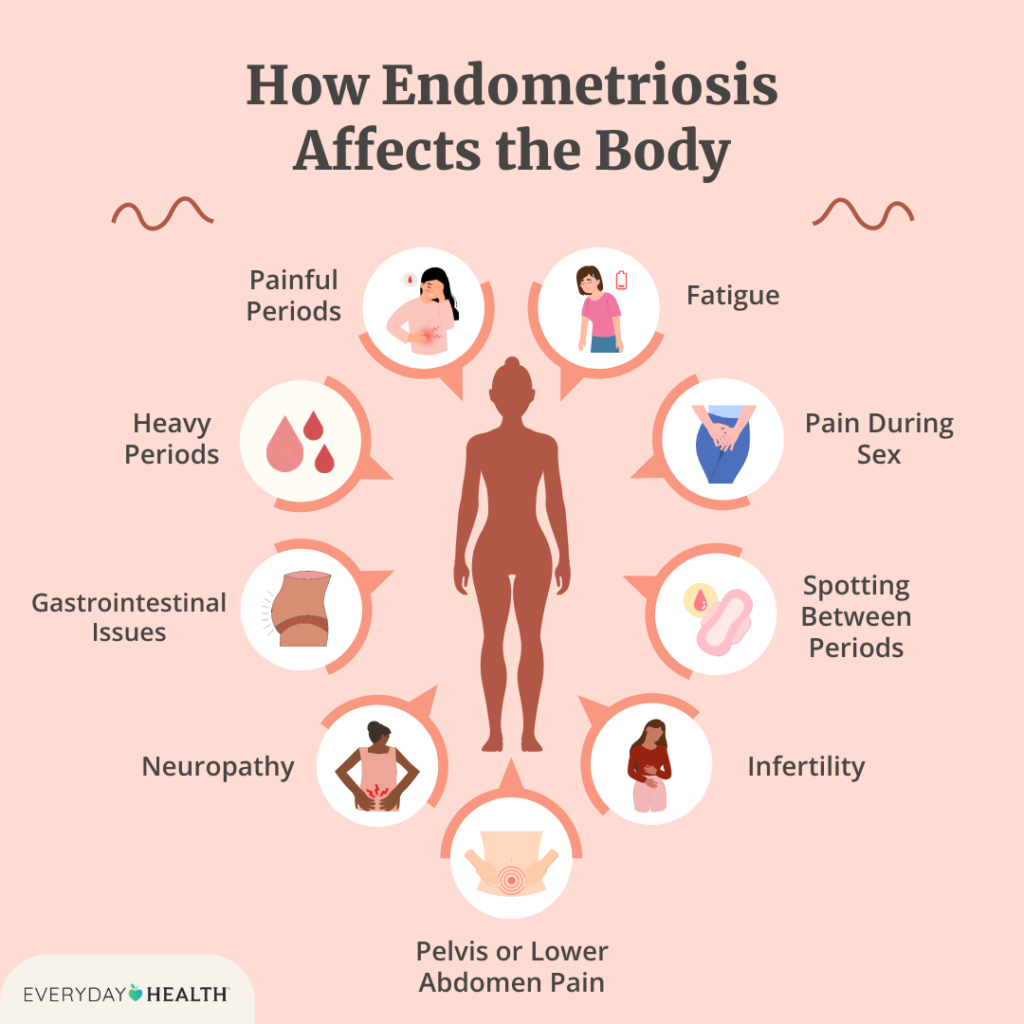
Symptoms of endometriosis
The symptoms of endometriosis can vary greatly between individuals, but common signs include:
- Pelvic pain: Often worse during menstruation but can occur at any time.
- Heavy menstrual bleeding or bleeding between periods.
- Pain during intercourse: Many women with endometriosis experience deep pelvic pain during or after sex.
- Bowel and bladder problems: Pain during bowel movements or urination, especially during menstruation.
- Fatigue and exhaustion: The chronic pain and physical toll of the condition can leave women feeling constantly tired.
- Infertility: Endometriosis is a common cause of infertility, although many women with the condition can still conceive.
The many manifestations of endometriosis inf affected women
Common myths and misconceptions about endometriosis
There are several misconceptions about endometriosis that often prevent timely diagnosis and effective treatment:
Myth No 1: Endometriosis is just “bad period pain.”
Reality: While period pain is a common symptom, endometriosis is much more than that.
It can cause severe, chronic pain that can be debilitating and occurs outside of menstruation as well.
Myth No 2: Endometriosis can be cured by pregnancy.
Reality: While some women report symptom relief during pregnancy due to hormonal changes, it is not a cure.
Symptoms often return after pregnancy.
Myth No 3: Hysterectomy (removal of the uterus) is a guaranteed cure.
Reality: Removing the uterus does not guarantee the elimination of endometriosis because the condition can occur outside the uterus. This option may provide relief in some cases but is not always effective.
Myth No 4: Endometriosis only affects older women.
Reality: Endometriosis can affect women of all ages, including teenagers. It’s crucial for young women experiencing severe menstrual pain to seek medical advice early.
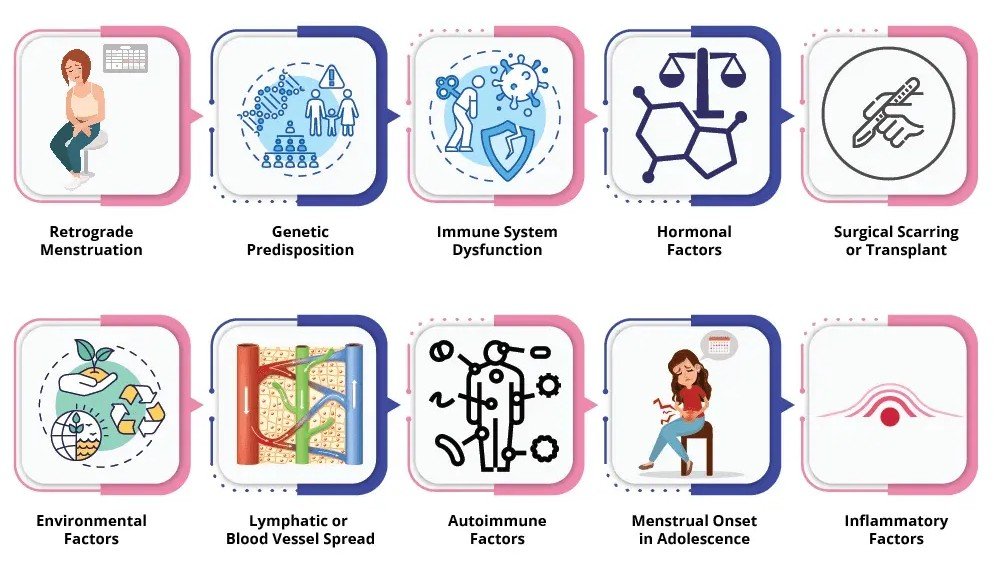
Causes of endometriosis
The exact cause of endometriosis is still unclear, but several theories exist:
- Retrograde menstruation: Menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body.
- Immune system disorders: An impaired immune system may fail to recognize and destroy endometrial-like tissue outside the uterus.
- Genetics: Women with close relatives (mother or sister) who have endometriosis are at higher risk.
- Hormonal imbalance: Estrogen, the hormone that regulates the menstrual cycle, plays a key role in the development of endometriosis.
The many possible causes of endometriosis
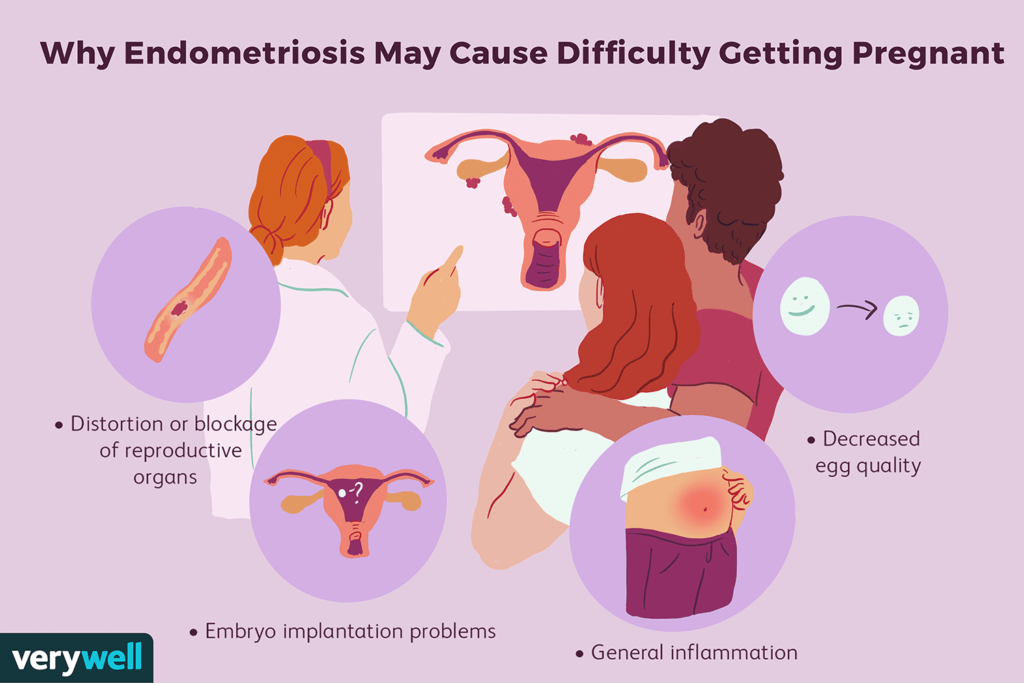
The impact of endometriosis on woman's fertility
Endometriosis can affect fertility in several ways, including:
- Scar tissue formation: The endometrial growths and resulting inflammation can cause scarring (adhesions) that block the fallopian tubes, making it harder for eggs to meet sperm.
- Ovarian cysts: Cysts called endometriomas can form on the ovaries, negatively affecting their function.
- Inflammation: Chronic inflammation in the pelvic area may disrupt the environment needed for fertilization and implantation.
While endometriosis can make it more challenging to conceive, many women with the condition can still get pregnant either naturally or with the help of fertility treatments.
The impact of endometriosis on fertility
How is endometriosis diagnosed?
Diagnosing endometriosis can be challenging because its symptoms often overlap with other conditions such as irritable bowel syndrome (IBS) or pelvic inflammatory disease (PID).
The following steps are typically taken to diagnose endometriosis:
- Medical history and symptom review: Your doctor will ask about your symptoms, menstrual cycle, and any family history of the condition.
- Pelvic exam: A physical exam may help identify cysts or scar tissue, but small areas of endometriosis may not be detectable.
- Imaging tests: Ultrasound or MRI scans can help identify cysts associated with endometriosis, but they may not detect all growths.
- Laparoscopy: The only definitive way to diagnose endometriosis is through laparoscopy, a minimally invasive surgical procedure that allows doctors to view and possibly remove endometrial tissue.
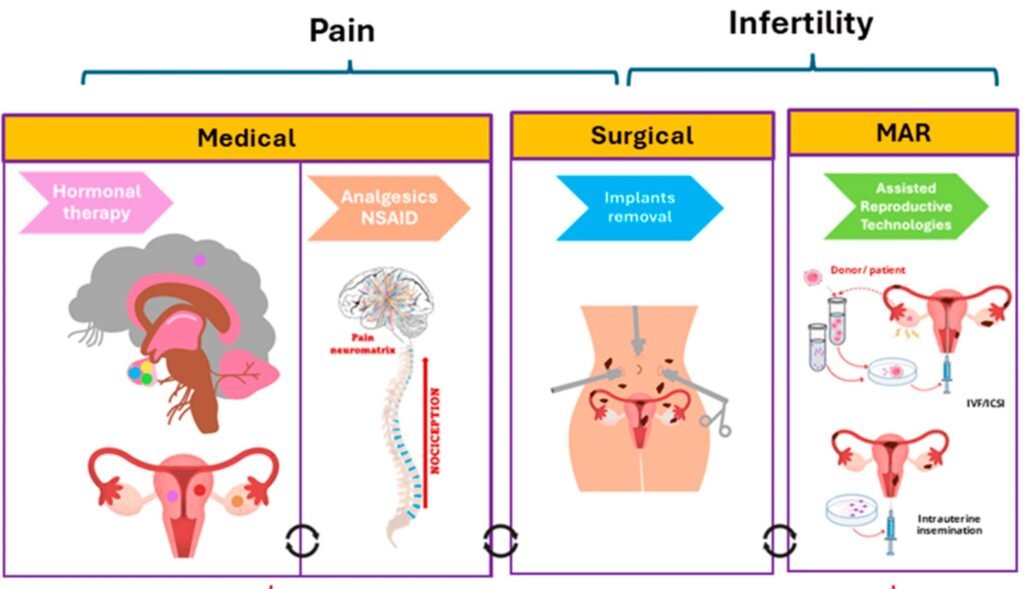
Treatment options for endometriosis - What can be done?
While there is no cure for endometriosis, several treatment options can help manage symptoms and improve quality of life:
- Pain management: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen can help reduce pain and inflammation.
- Hormonal therapies: Birth control pills, hormonal IUDs, or medications that reduce estrogen levels can help control the growth of endometrial tissue and alleviate symptoms.
- Surgical treatment: Laparoscopic surgery can remove or reduce endometrial growths, improving pain and fertility. However, recurrence is possible, and surgery is not a permanent solution.
- Fertility treatments: For women struggling with infertility due to endometriosis, assisted reproductive technologies like in vitro fertilization (IVF) can be helpful.
Summary of management options for endometriosis – For pain and infertility
Living with endometriosis: Coping strategies
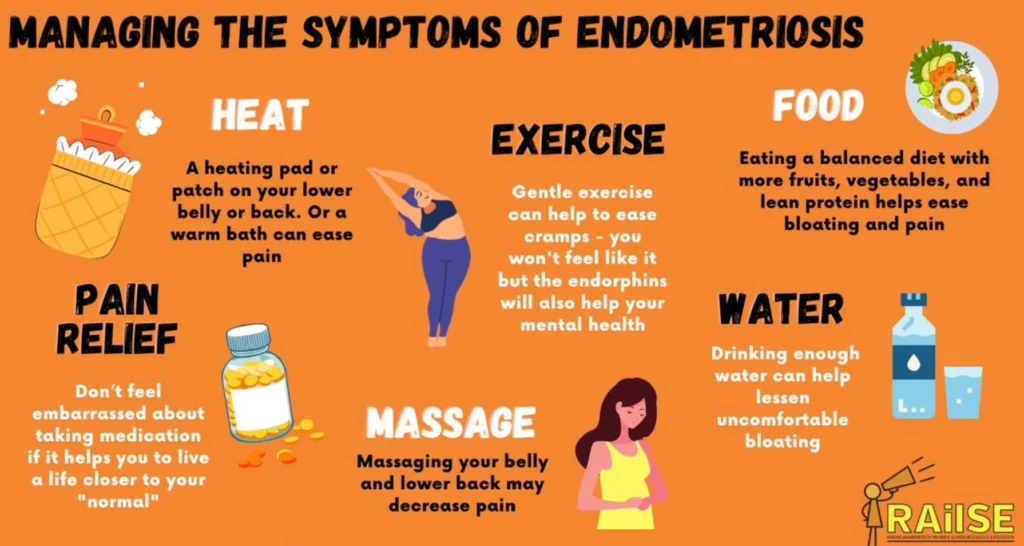
Endometriosis is a lifelong condition, and many women find that they need to make lifestyle adjustments to manage their symptoms. Here are some tips for coping with endometriosis:
- Track your symptoms: Keeping a journal of your pain and other symptoms can help you and your doctor track patterns and find the most effective treatments.
- Adopt a healthy diet: Some women find that reducing inflammatory foods (like processed foods and red meats) and increasing anti-inflammatory foods (like fruits, vegetables, and omega-3-rich foods) help reduce symptoms.
- Practice stress management: Endometriosis can take a toll on mental health. Techniques such as yoga, meditation, and counseling can help manage the emotional impact.
- Join a support group: Connecting with others who understand your experience (including online) can be empowering and provide practical advice for managing symptoms.
Tips for coping with endometriosis
A piece of advice: Being realistic about treatment outcomes
While treatments can provide significant relief, endometriosis is a chronic condition that often requires long-term management.
Some women experience recurring symptoms even after surgery or medical treatments.
It’s therefore important to have open discussions with your healthcare provider about what can realistically be achieved, including the possibility of needing ongoing treatments.
Remember
Endometriosis is a complex and often misunderstood condition that can significantly impact a woman’s physical, emotional, and reproductive health.
By dispelling myths and providing clear information, we can help more women get the diagnosis and treatment they need.
While there is no cure, effective management can greatly improve quality of life, allowing women to live healthier, more fulfilling lives.


